Wow, have we ever been there, and breastfeeding is not for the faint of heart. We have 8 children between us and, in our homes, we have nursed exclusively, nursed and done bottles and done bottles only. We have also had the opportunity to work with thousands of families on their feeding journey through our on-call days at a very busy pediatric office and through our personal consulting services over the last 20+ years serving families in 6 continents (sorry, Antarctica).
Breastfeeding Basics: Preparation
Reading books, taking classes (private or hospital-based), and knowing your goals are all great to do while preparing for the arrival of your little one. However, know that we can have the best-laid plans and we can have done “all” the things; yet our plans may still not go perfectly. This is normal, and you will need to give everyone grace (your little one(s) AND yourself included).
- Define your goals (Note: These can change and sometimes may change by the minute)
- How long would you like to breastfeed exclusively?
- Will you want to introduce occasional bottles?
- Will you be staying at home for the first year?
- Will you be working from home?
- Will you be heading back to work and going to daycare or getting a nanny?
- Create and share your goals with your healthcare provider and partners.
- Take breastfeeding classes in person, hospital, and/or online (look for a lactation consultant that will listen and help you with your goals).
- Gather essential items to have on hand: (here are a few of our favs)
- High-Quality Breast Pump
- Nursing Pillow (or two)
- Nursing Bras and Tops
- Breast Pads
- Storage Bags
- Nipple Cream
- Haaka
- Nipple Shield
-
3-Tier Rolling Cart (above items that fit) plus:
- Snacks
- Water
- Phone Charger
- Diapers and Wipes
- Burp Cloths
- Choose your support system. Include your people in your plans/goals. How can they help?
- Preparing meals
- Helping with positioning
- Getting that little one awake, changed, and ready to eat.
- Washing supplies and helping to clean up
The First Few Weeks
We will say it again and again, give yourself grace. (In fact, Laura Hunter always encourages us to be “Grace in the Chaos”. You will see this emblazoned on some tee-shirts and in the hearts of moms all over the world!). The first few weeks will consist of everyone learning something new!
- Breasts (especially the nipples) may have some soreness. This should get better within 7-10 days. If severe pain and/or no improvement, then connecting with your MOC Premier Consultant, lactation consultant, and/or pediatrician can help. We want to ensure a good latch, that the baby is not tongue or lip-tied, and that you are enjoying the correct feeding positions and support.
- You will feed every 2-3 hours for the first 2 weeks or so. It takes a few days and sometimes up to a week for that milk to be “in,” and you will know when that happens (sometimes due to weight loss, medications, recovery, or preference: supplementing may be advised or warranted). This is okay!
- Your little one may be sleepy when it is time to feed. Here are a few things to try
- Nurse the baby in a diaper only
- Tickle/Stroke bottoms of feet
- Change breastfeeding position
- Burp
- Change diaper
- Cool cloth on baby's face, neck, or feet
- Relatch by breaking suction (slipping finger in the side of mouth and turning finger) and repositioning on the breast. Then, try to get the nipple and areola in the mouth.
- Once your milk is in, your feeding experience will evolve to let your focus be on emptying the first breast and then moving to the 2nd. You can tell that it is empty typically by how it “feels.” Make sure it is soft and mushy, then burp, give a break, and offer that second breast. We call the 1st breast the ‘entree’ and the 2nd breast ‘dessert.’
Breastfeeding FAQs
When can we start a routine if we are breastfeeding?
You can start the MOC routines once the baby is 2 weeks of age and past birth weight. Feeding about every 2 hrs and 45 mins to 3 hours typically during the day, then “on-demand” at night (meaning we let them determine when they eat during the night). This typically results in gradually getting longer stretches of sleep n a row at night as they increase their intake during the day. You may have two feeds, one feed, or even three feeds (on the rough nights - sorry, but those do exist even at MOC - but not for long!).
When will my breastfed baby sleep through the night?
Typically with families using MOC, we begin to see:
- 5-6 hour stretches by 6-8 weeks of age (maybe not every night)
- 6-8 hour stretches with occasional through the nights by 8-10 weeks
- 10-12 hours by 3 months of age
They all grow, and they are moving forward healthy and well cared for by moms and healthcare professionals - yes, even breastfed babies- literally thousands of them).
Will it hurt my supply to let them sleep as long as they want to at night?
Your body is a great example of supply and demand. If your little one has gradually gone longer stretches at night, then they will suck differently during the day, and your body will increase to what they need. Your breasts may not feel as full as they get more efficient, and your body makes the adjustments.
If you are ever concerned with supply and/or weight gain, then work with your MOC Consultant, lactation consultant, and/or pediatrician to achieve your goals and ensure proper weight and growth.
How to tell the difference between engorgement, blocked ducts, thrush, or mastitis?
- Engorgement: Full breasts that turn hard and painful.
- Ensure proper latch
- Empty breast massage while nursing
- You may need to manually pump before nursing to soften it slightly
- Blocked Ducts: This is very common and is a tender sore lump, usually in one breast. This happens when the duct is not emptied well.
- Ensure proper latch
- Massage area while nursing
- Warm compresses while nursing on the area
- Supportive bra (not tight)
- Mastitis: You feel as if you have been hit by a truck! Typically soreness, redness to breast, fever, flu-like symptoms, may have nausea/vomiting, warm breast.
- Call your doctor immediately- as there may be some medications needed to help with the infection.
- Ensure proper latch
- Massage the area behind the soreness, making a circular motion and moving toward the nipple.
- Supportive bra (not tight)
- Thrush/Fungal infection: Overgrowth of Candida. Nipple soreness for a few days, redness around the nipple, pain that shoots up the breast. Shiny, itchy nipples.
- Call the doctor with your symptoms.
- Clean nipples with a vinegar wash (2 parts water to 1 part vinegar)
- Wash gently with warm water prior to nursing.
- Change nursing pads often.
- Wash clothes in hot water.
- Boil bottle nipples, pacifiers, and pump parts and/or replace them after 3-4 days of treatment.
- Check the infant for thrush-white patches on the inside of cheeks and/or lips that do not wipe off with your fingernail.
ALWAYS contact your medical professional to discuss your plan of treatment
Remember, at the end of the day, we want you to feel supported through your feeding experience. You are the best one to decide what works in your home at this particular season of your life with this baby, and we are here to help with whatever your feeding journey may look like. Fed is best, and there isn’t just one way to do that. There is nothing more wonderful for us than helping families find what works for them! Don't compare yourself to others. Find what works for YOU and your little one.
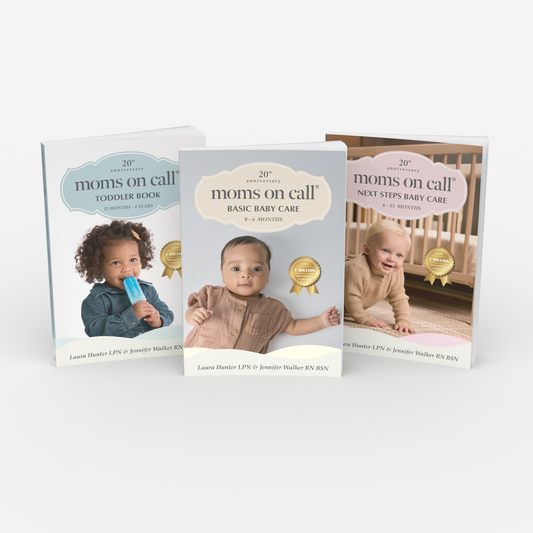
Follow along in the Book and Online Courses for all things Moms on Call!